Tailbone pain (Coccydynia): What, why, and how it’s diagnosed
*This article has been written at a basic level, so that everyone can understand it.
For what you can do about Coccydynia, see my following article on treating Coccydynia. https://www.drcarpino.com/blog/tailbone-pain-coccydynia-self-management-and-how-its-treated
Tailbone pail (also known as Coccydynia, or Coccygodynia) is pain coming from the very bottom of your spine.
The coccyx is at the bottom of the spine. Even though it is small, a painful coccyx can cause widespread pain.
It attaches to the sacrum bone above it by 3 joints. The entire coccyx is otherwise fused in adults and moves as a single unit. Most of the pelvic floor muscles attach to the coccyx, and other common pain generating muscles are generally close as well. These muscles include your hip flexor muscles, your gluteal muscles, and low back muscles.
In front of the coccyx sits the Ganglion Impar. Basically, it’s the location of the nerve cell bodies which serve the surrounding area. This is a structure which can be targeted during coccydynia treatments as well.
Coccyx bones come in a variety of shapes and sizes. In general, the sharper the angle that the coccyx points forward, the more prone the structure is to becoming a pain generator. Take a look here if you’d like to visualize this: https://radiopaedia.org/articles/anterior-angulation-of-the-coccyx. Sometimes small bony bumps (called spicules) form on the coccyx and are painful to touch too.
The function of the Coccyx is to: (i) be an attachment site for muscles and ligaments, (ii) positional support for the anus, (iii) acting as one of the “legs of the tripod” for seated weight bearing (the other two legs are part of your pelvis- the Ischial tuberosities).
According to the scientific literature, the risk factors for developing coccyx pain include: (i) being female, (ii) greater body weight, (iii) prolonged sitting, (iv) sharper forward angle of the coccyx (like we said above). The process of childbirth is suspected to be related to coccydynia. Like most aches and pains, tailbone pain is likely underreported in males since males seek less care for these kinds of things.
It is unknown what percentage of the general population has coccydynia on a daily basis.
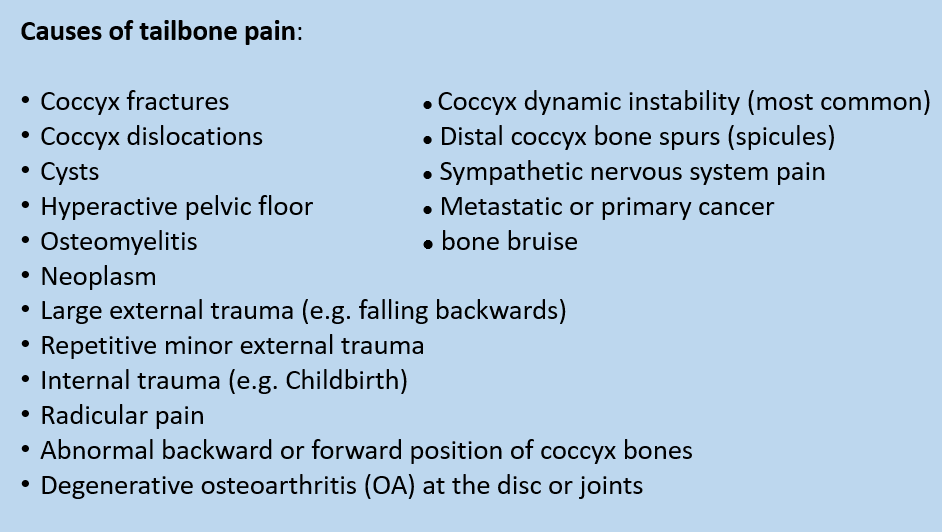
In no particular order, here is the list of almost everything that can cause tailbone pain:
Don’t worry if these words are confusing. It’s your doctor’s job to explain if any of them are meaningful to you.
Most cases of Coccydynia resolve by themselves without needing to see a doctor in the first 3-6 months from it’s onset.
Coccydynia is both a symptom and a diagnosis. Diagnosing Coccydynia comes from a conversation on the history of the discomfort and a physical exam which determines which structures are involved. Diagnostic imaging such as X-rays are occasionally obtained to advise your doctor on how to better treat the pain.
Some common symptoms I hear from people with tailbone pain include: pain with sitting, pain from leaning backwards, pain with standing up, pain standing up for a long time, other pains in the low back or buttocks (due to the body compensating), and possible pains from intercourse or passing stool.
The physical examination of coccydynia begins with explaining what needs to be touched and why, and how the procedure is performed. Even though I am a pretty excellent doctor, no matter how well I explain this process it’s always somewhat awkward the first time for yourself as a patient ¯\_(ツ)_/¯ . If you consent to physical examination, I investigate: how you walk, the surrounding muscles, ligaments, and joints of the low back and hips, I look at the painful area, and perform precise coccyx palpation (external). Depending on the shape of your particular coccyx, internal palpation may or may not be necessary. If a finger joint needs to be inserted into the anus for the purpose of physical examination, I check for appropriate coccyx-sacrum joint movement and overactive pelvic floor muscles.
If your doctor is confident in the diagnosis of Coccydynia then they will recommend manual therapy from a trained and experienced Chiropractor in this field. Typically, a trial of care is performed to see if the pain can be resolved before proceeding with further medical processes, since 90% of Coccydynia patients are successfully treated at this step. Your doctor may ask you to receive X-rays or other imaging if they think that the results of the imaging will effect their method of treating the pain.
In my following article on Tailbone pain, I will explain in detail the steps and options for treating coccydynia including: do-it-yourself methods, what a Chiropractor can do, and what medical specialists can do.
References:
1.Bogduk, N.. Ganglion impar blocks for coccydynia: a case series prerequisite for efficacy trial. Pain Med. 2015. 16(7):1245
2.Foye, P. Coccydynia: Tailbone pain. Phys Med Rehab Clin of N Am. 2017. 28(3):539-49
3.Foye, P. et al. Tailbone pain from coccyx injuries on waterslides: a case series. J Emerg Med. 2018. 55(2):e33-e35
4.Kodumuri, P., Raghuvanshi, S., Bommireddy, R., Klezl, Z. Coccydynia- could age, trauma, and body mass index be independent prognostic factors for outcome of intervention? Ann Royal Coll Surg Engl. 2017. 100(1):12-15
5.Lirette, LS., Chaiban, G., Tolba, R., Eissa, H. Coccydynia: An overview of the anatomy, etiology, and treatment of coccyx pain. 2014. Ochsner J. 14(1):84-7
6.Maigne, JY., Chatellier, G. Comparison of three manual coccydynia treatments: a pilot study. Spine. 2001. 26(20):e479-83
7.Marinko, L, Pecci, M. Clinical decision making for the evaluation and management of coccydynia: 2 case reports. J Ortho & Sports Phys Ther. 2014. 44(8):615-21
8.Mohanty, P., Pattnaik, M. Effect of stretching piriformis and iliopsoas in coccydynia. J Body Mov Ther. 2017. 21(3):743-746
9.Scott, K., Fisher, L., Berstein, I., Bradley, M. The treatment of chronic coccydynia and post coccygectomy pain with pelvic floor therapy. PM R. 2017. 9(4):367-76